
Anti-Inflammatory Diet & Pyramid
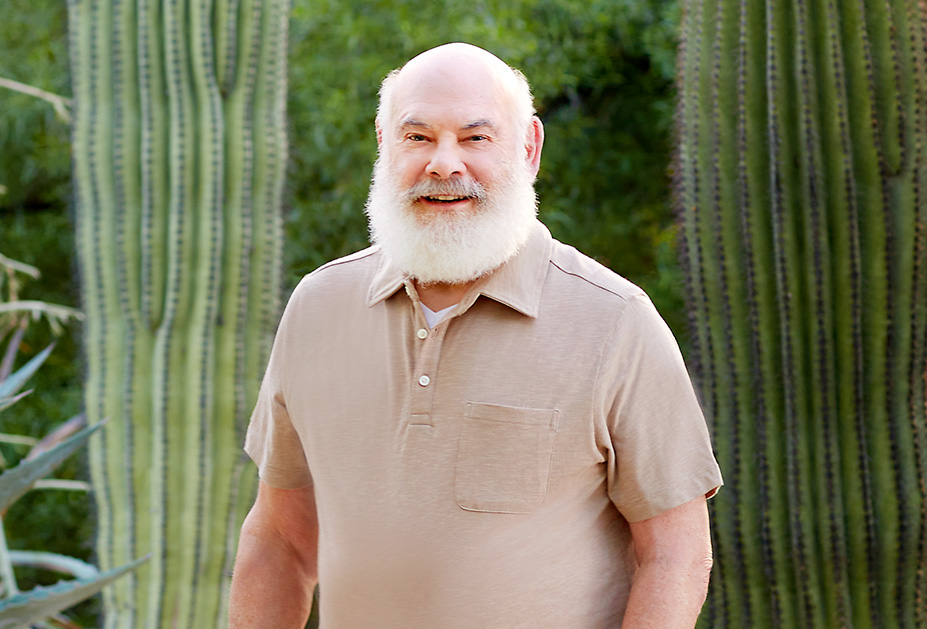
Dr. Weil's Anti-Inflammatory Food Pyramid
Mouse over the sections in the interactive pyramid above for more information! Learn more about Dr. Weil’s…
about Dr. Weil's Anti-Inflammatory Food Pyramid



What can you tell me about calcium aspartate anhydrous? I’ve read that it has the highest rate of…